CLINICAL GOVERNANCE
The care quality commission states that clinical governance is a systematic approach to maintaining and improving the quality of patient care. It provides a framework for drawing together the different strands of quality improvement which includes clinical audit, clinical leadership, evidence-based practice and the dissemination of good practice, ideas and innovation and addressing poor clinical performance.
All healthcare providers should give clinical governance a high priority. It should be led by senior members of the practice who understand their responsibilities to improve the quality-of-care patients receive and are accountable for the quality of clinical practice provided by clinicians in the practice. All staff members should be involved.
Regulation 17 of the CQC clinical governance requirements states the following:
- Systems or processes must be established and operated effectively to ensure compliance with the requirements in this Part.
- Without limiting paragraph (1), such systems or processes must enable the registered person, in particular, to:
- Assess, monitor and improve the quality and safety of the services provided in the carrying on of the regulated activity (including the quality of the experience of service users in receiving those services);
- Assess, monitor and mitigate the risks relating to the health, safety and welfare of service users and others who may be at risk which arise from the carrying on of the regulated activity;
- Maintain securely an accurate, complete and contemporaneous record in respect of each service user, including a record of the care and treatment provided to the service user and of decisions taken in relation to the care and treatment provided;
- Maintain securely such other records as are necessary to be kept in relation to:
- Persons employed in the carrying on of the regulated activity, and
- The management of the regulated activity;
- Seek and act on feedback from relevant persons and other persons on the services provided in the carrying on of the regulated activity, for the purposes of continually evaluating and improving such services;
- evaluate and improve their practice in respect of the processing of the information referred to in sub-paragraphs (a) to (e).
- The registered person must send to the Commission, when requested to do so and by no later than 28 days beginning on the day after receipt of the request:
- a written report setting out how, and the extent to which, in the opinion of the registered person, the requirements of paragraph (2)(a) and (b) are being complied with, and
- any plans that the registered person has for improving the standard of the services provided to service users with a view to ensuring their health and welfare.
7 PILLARS OF CLINICAL GOVERNANCE
As part of these arrangements our principles and processes are underpinned by the 7 pillars of clinical governance:
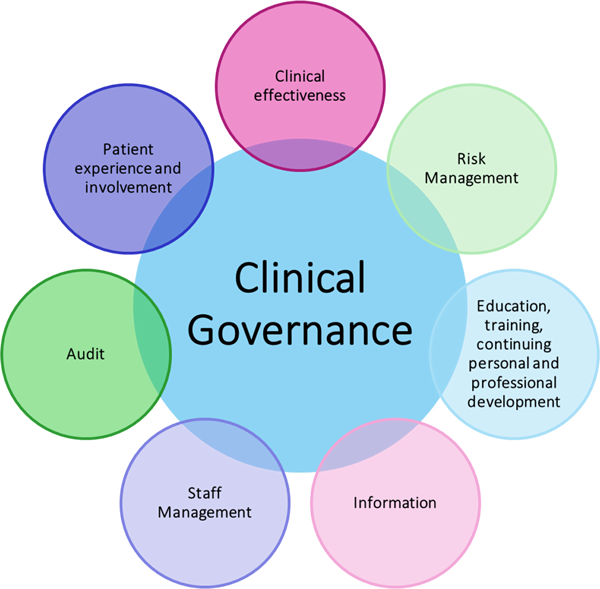
Patient-centred care is the cornerstone of clinical governance. This pillar stresses the importance of involving patients in decision-making processes, respecting their preferences, and promoting effective communication between healthcare providers and patients. By adopting a patient’s perspective, we can tailor their services to meet patient needs and enhance the overall quality of care.
Pillar
2
Clinical Effectiveness
Clinical effectiveness is focused on providing evidence-based care that leads to positive outcomes. This involves applying best practices, tracking treatment results, and continuously evaluating clinical processes. By integrating the latest research and medical advancements into daily practices, we can ensure that its services are both current and effective in improving patient health.
Pillar
3
Patient Safety
Patient safety is the top priority for us. This involves implementing robust reporting systems for adverse events, conducting regular risk assessments, and adhering to safety protocols. A culture of transparency and accountability is crucial for preventing errors and ensuring patient safety.
Pillar
4
Governance and Leadership
Strong leadership and governance are essential for the success of clinical governance within our organisation. This pillar focuses on establishing clear lines of responsibility, promoting leadership development, and ensuring that the organisational structure supports the delivery of high-quality care.
Pillar
5
Information Management
In today’s digital age, the effective management of information is critical for providing quality and improvement in healthcare. This pillar involves implementing robust information systems to collect, analyse, and disseminate data relevant to patient care. Accurate and timely information enables healthcare providers to make informed decisions, track performance, and identify areas for improvement.
Pillar
6
Training and Education
Ongoing training and development of healthcare professionals are central to clinical governance. This pillar recognizes the dynamic nature of healthcare and the need for continued learning to stay ahead of changes in the sector. Continuous learning ensures that we are equipped with the knowledge and skills necessary to deliver high-quality, up-to-date care.
Pillar
7
Performance and Monitoring
The final pillar of clinical governance involves establishing mechanisms for performance monitoring and quality and improvement. Regular audits, reviews, and evaluations allow us to assess their performance against established standards. By identifying areas of strength and areas needing improvement, we implement targeted strategies to enhance the overall quality of care.
CONTACT US TODAY
Connect with qualified specialists through our quick and streamlined online or face to face assessment process.
Experience the perfect blend of expertise and convenience.